No More Waiting Weeks for Approvals
Accelerate Your Prior Authorizations
Speed up your approval process with the power of AI, smart automation, and extensive payer integrations. XyberMed’s Patient Access Plus Prior Authorization Module streamlines requests, reduces delays, and ensures faster approvals—helping your practice deliver care without unnecessary hold-ups.
OUR SOFTWARE + OUR SPECIALISTS = COMPLETE COVERAGE
Your Prior Authorizations
Fully Managed by Our Expert Team
Navigating prior authorization can be complex, time-consuming, and a barrier to timely patient care. XyberMed’s AI-powered Patient Access Plus platform transforms this process—reducing delays, eliminating inefficiencies, and streamlining approvals.
Our solutions integrate seamlessly into your existing workflows, delivering accuracy, speed, and scalability so your team can focus on what matters most—providing exceptional care to your patients.
Proven Performance with XyberMed
prior authorization accuracy rate
average turnaround times for standard procedures
denial rate
increase in cost efficiency for your organization
boost in your staff’s productivity
AUTHORIZATION DETERMINATION ENGINE
Shortlist Which Cases Need Authorization Instantly
Leverage the power of AI and extensive integrations with clearinghouses and benefit managers to instantly check if prior authorization is required for patient care.
Accurate Determination
Our advanced authorization determination engine automatically checks payer guidelines and CPT codes with over 98% accuracy, letting you know immediately whether an authorization is needed.
Instant Notifications
When no authorization is required, the status is instantly updated in your EMR, and your staff is notified right away—saving valuable time.
More Appointments, Less Admin Work
This feature alone has helped our clients schedule more procedures and save hours of manual work reviewing payer rules—boosting both efficiency and revenue.
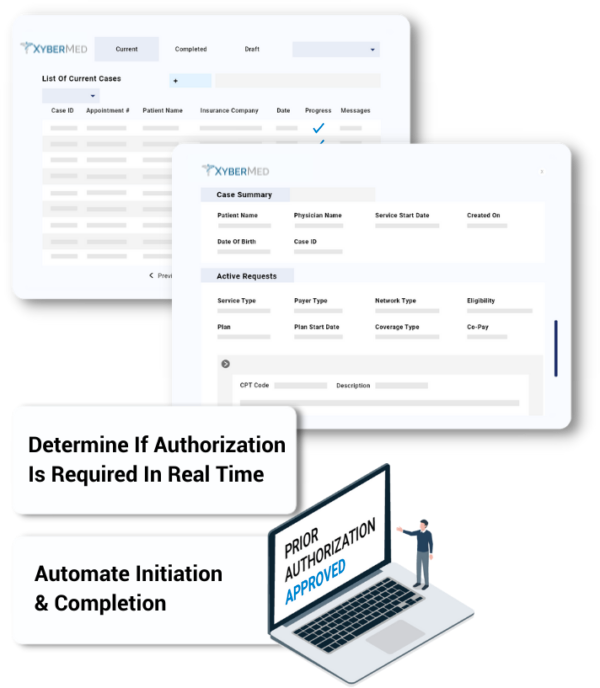
ELECTRONIC AUTHORIZATION SUBMISSIONS
Automate Initiation, Checks & Updates
Navigating prior authorization processes can be tedious and time-consuming, leading to delays in patient care and operational inefficiencies. We optimize the way healthcare providers handle prior authorizations with our AI-powered platform, Patient Access Plus.
Our solutions are tailored to your existing workflows and are designed to deliver accuracy, speed, and scalability, ensuring that providers can focus on delivering exceptional patient care.

PRIOR AUTHORIZATION ANALYTICS
Leverage Real-Time Data to Gain Actionable Authorization Intelligence
Gain complete visibility into your prior authorization process with detailed, real-time analytics and reporting—all in one powerful dashboard.
Comprehensive Dashboard
View up-to-the-minute data with real-time updates. Apply custom filters to focus on the insights that matter most to your practice.
Actionable Insights
Leverage predictive analytics to understand usage trends, optimize workflows, and address potential bottlenecks before they impact patient care. Reduce claim denials caused by prior authorization issues and keep your revenue cycle running smoothly.

Automation Agents Built For
Prior Authorization









Looking to Accelerate Prior Authorization Approvals?
At XyberMed, our AI-powered patient access solution streamlines the prior authorization process—reducing delays, minimizing denials, and improving patient care.

Compatible With Most EMRs
At XyberMed, we offer bi-directional integration with most leading EHR, EMR, LIS, and RIS platforms. Whether your system supports API, HL7, FHIR, X12, or uses an EMR developer program, our solutions are built to work smoothly with your existing infrastructure.









